Managing Gum concerns at SHDC

Our hygienists, Leean, Jess, Emily and Rachelle are our resident experts in gum disease and the first line in diagnosing and managing this condition. During your visits with them they will discuss the prevention of gum disease with you. If the gum disease is very severe, your dentists will refer you to a periodontist, a dentist specialising in gum disease management, for a course of care to stabilise the disease.
Gum Disease – As outlined by the ADA
Periodontal diseases are a wide range of diseases that affect the gums. The most common types of periodontal disease are gingivitis and periodontitis.
Gingivitis
Gingivitis is the mildest and most common form of periodontal disease. Inadequate oral hygiene causes accumulation of dental plaque at the junction of the tooth and the gum (Figure 1B). As a result, the gums become inflamed, with common visual signs being redness, swelling, and bleeding. There is usually little or no discomfort at this stage. However, bleeding gums are a sign of disease, as healthy gums do not bleed, and this can lead to more serious problems. Gingivitis is reversible with professional tooth cleaning and good regular oral care at home, so it is important to seek professional assessment if gum bleeding is detected during brushing or eating.
Periodontitis
When gingivitis is unable to be controlled the inflammation progresses to periodontitis, a common chronic disease that affects at least 25% of the adult population. Periodontitis is caused by dental plaque that contains destructive bacteria that result in the loss of the supporting structures around the teeth (gum and bone) (Figure 1C-Figure 1D). This causes the formation of ‘pockets’ around the teeth and/or recession of the gums. As is the case with gingivitis, inadequate oral hygiene is a risk factor for periodontitis, as are various systemic diseases (eg diabetes) and harmful habits (eg smoking). Genetic predisposition is a major contributor to the risk of developing periodontitis, and patients with a family history of periodontitis should have their gum health closely monitored.
Although periodontitis is not usually painful, common signs of the disease include gum recession (ie. ‘getting long in the tooth)’ and mobility (loosening) of the teeth. If untreated, periodontitis may result in the loss of teeth. With appropriate professional care the condition can usually be stabilised.
Latest Articles Answering Your Common Questions
Looking for a dental partner who provides quality and care for you and your family?
Give us a call today on (08) 8278 6858 or complete the online form to book your appointment or discuss how we can help you with your dental care.
FAQs
Signs of gum disease include red, swollen, or bleeding gums, persistent bad breath, and loose teeth.
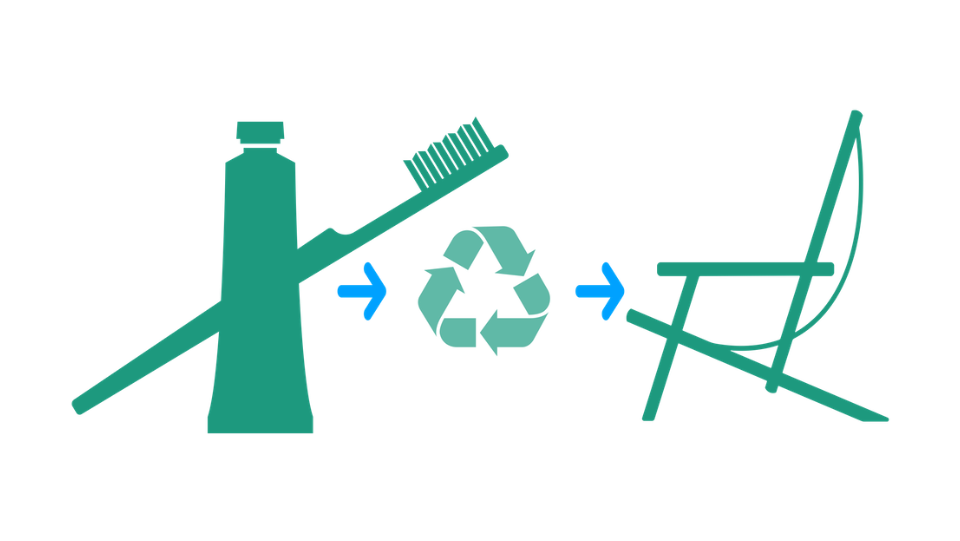
Maintain good oral hygiene by brushing and flossing daily, avoid tobacco use, and visit your dentist regularly for cleanings and check-ups.
Treatments range from professional cleanings and scaling and root planing to more advanced procedures like periodontal surgery, depending on the severity of the condition.
Dr Tharaka Narayana replies:
Yes, you possibly could, but it’s best to come in for a dental check-up to determine this for sure.
Gingivitis is very prevalent. Many of us will experience this condition – mild inflammation of the gum – at least once in our lives.
Getting on top of it with preventive dental care is important in making sure it doesn’t progress to periodontal disease – which, worst case scenario, can result in someone losing their teeth.